From tracking sleeping patterns to counting steps and physical activity, people across Wales have been using technology on their smartphones to monitor health and wellbeing for some time. However, such digital tools also have the potential to help the nation measure more clinical metrics.
From tracking sleeping patterns to counting steps and physical activity, people across Wales have been using technology on their smartphones to monitor health and wellbeing for some time. However, such digital tools also have the potential to help the nation measure more clinical metrics.
Indeed, our health and social services have started evaluating the impact and benefits of such an approach. The adoption of technology was accelerated by the initial reaction to the Covid-19 pandemic, where health and social care practitioners rapidly adapted and digitised services. Tools such as video consultations and digital triaging were employed to ensure patient needs were still being met while complying with social distancing rules.
The DSF supported this immediate response and continues to do so. The £150,000 Welsh Government initiative, coordinated by DHEW, focuses on rapidly deploying and testing digital technologies to explore alternative ways of supporting the needs of our health and social care systems following COVID-19.
This includes a pilot in Cwm Taf University Health Board and Betsi Cadwaladr University Health Board using digital tools developed by our organisation, Huma. We have created remote patient monitoring (RPM) technology that allows patients and practitioners to remotely manage long-term and chronic conditions.
We have already deployed this technology as a COVID-19 solution in Germany, and 15 NHS organisations are using it to manage other conditions. This pilot presented an ideal opportunity to evaluate its effectiveness in helping patients and practitioners manage heart failure conditions – which typically require extended stays and repeated visits into hospitals.
Proactively managing and monitoring heart failure
We kicked off the 12-week pilot on Monday 12th July across both Health Boards, with the objective of determining whether RPM can help improve experience, care, outcomes and efficiency for those experiencing and treating heart failure.
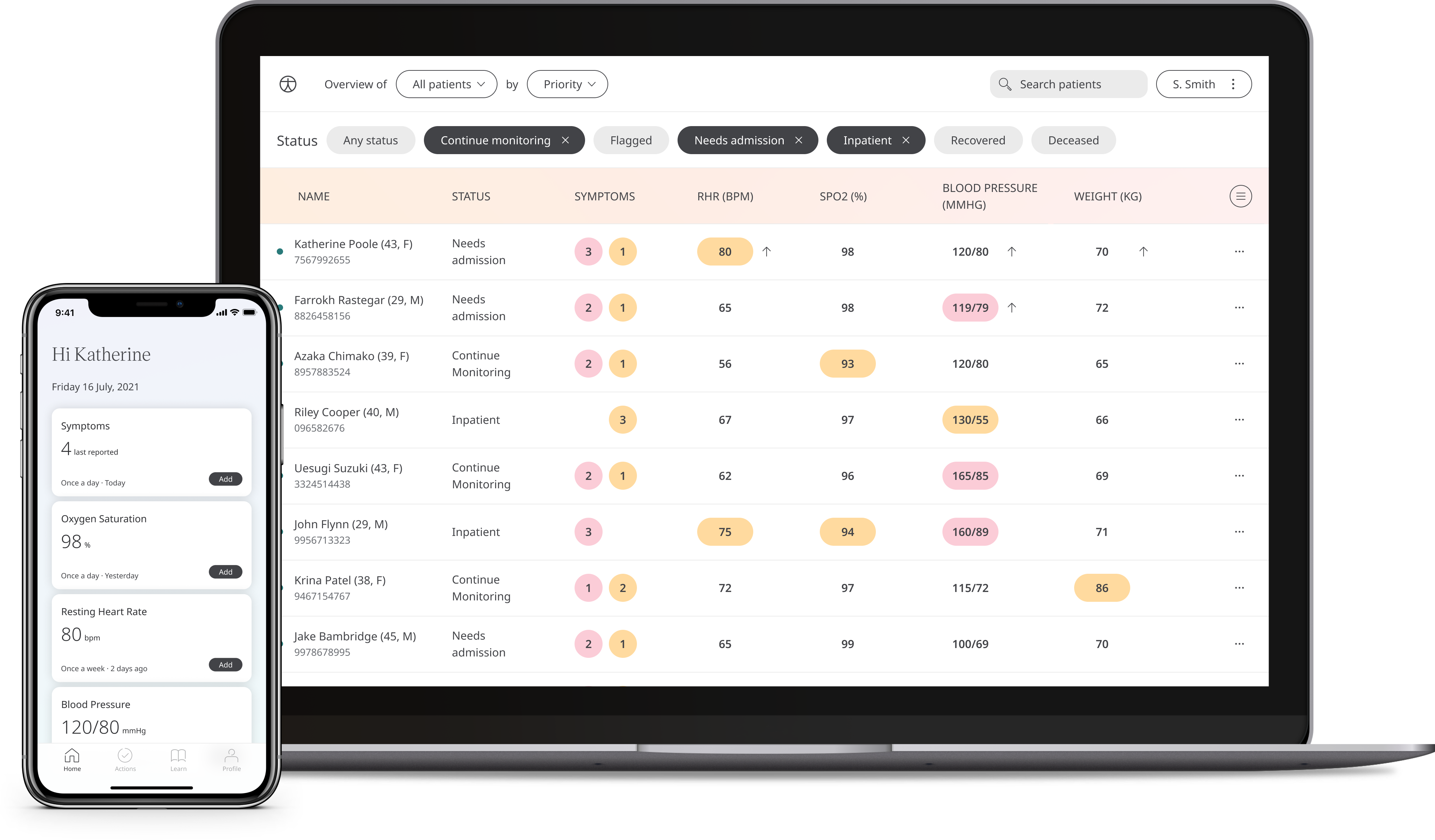
The pilot has seen a cohort of patients monitor their conditions using a smartphone Patient App and equipment such as a pulse oximeter and blood pressure cuff. Data including symptoms, heart rate, blood pressure, oxygen saturation and weight can be uploaded in the comfort of the patient’s home.
Clinicians can then access this information in real time using a web browser portal. Here, they can use this data to make decisions about patients, spot early signs of health deterioration, and contact patients using built-in video consultation and telemedicine tools.
This removes the need for patients to travel into hospital or a primary care setting, which many would rather avoid as it is easier and saves on transport costs. It also helps to ease capacity and provide clinicians with a good line of sight on who they are treating.
The story so far
Both Health Boards are already seeing some very positive outcomes. For patients it means that they can be discharged from hospital earlier as they can be safely monitored from home. Their feedback has been positive, as all enrolled found that the software was helpful for improving clinician communication and managing their heart condition. Patients commented that the app was easy to use and helped put them in control of their health.
The project has also supported clinical teams’ efforts – mapping out patient progress and trajectories. This includes identifying patients who need extra tests, support, or earlier treatment before they attend planned appointments.
Looking to the future
Pilots like this provide a unique opportunity to understand best practices and learnings that can be applied in other digital healthcare projects moving forward. One of the lessons from this pilot is the importance of good internal communications. A weekly project meeting helped drive progress and engaging with clinical colleagues created a support and feedback forum.
It also demonstrated the critical role that the clinical team have had. Their engaged and enthusiastic response has helped to drive the pilot forward, setting the foundation for potential transformation.
The pilot also allowed the project team to identify key challenges that they may face if they want to continue with or scale up the project. One such way is streamlining information governance, which would accelerate the process by making it easier for Health Boards and NHS organisations to adopt this technology.
As the project draws to a close, we can see that the partnership between Huma, Cwm Taf Morgannwg University Health Board, and Betsi Cadwalladr University Health Board has already made a real difference to important patient outcomes while supporting clinical efforts and workflows.
We are delighted with the efforts that both Health Boards and all patients have put into making this project work and are keen to explore the opportunities for continuing this project.
To learn more about the projects coordinated or supported by DHEW then please visit the project page.
